

You’ve heard about chronic care management programs. But you’re uncertain what using one would mean for your clinic. Undoubtedly implementing a chronic care management (CCM) program will take time, staff, and money to name a few things—but what are the hidden challenges?
And what are the benefits of using an outsourced chronic care management program versus simply doing it all yourself?
Below we will delve into all aspects of CCM programs including what they are, their benefits and challenges, and a whole lot more.
Yes, it’s the industry’s most up-to-date guide—start finding all the answers to your questions, now!
Chronic care management (CCM) focuses on serving individuals on Medicare with two or more chronic conditions. CCM is a preventative service, helping your eligible Medicare patients take a proactive approach to their health and wellness, while keeping them connected to their provider.
According to recent statistics, 80% of chronic diseases could be eliminated by preventative measures. Also, two-thirds of all deaths in America are attributable to one of five chronic disorders: cancer, chronic obstructive pulmonary disease, diabetes, heart disease, and stroke.
A good CCM program can aid your clinic in facilitating earlier interventions among patients, encouraging compliance with medication regimens, supporting lifestyle improvements, and even reducing the number of hospitalizations, complications, and unnecessary ER visits that your patients may face.
A CCM program can provide help for patients who face at least two chronic conditions which are expected to last at least 12 months. Patients must consent to being in the program and each patient will require a care plan. Encounters must last at least 20 minutes each month and can go up to 60 minutes.
Should a patient’s conditions meet the proper criteria set forth by Medicare, they are eligible for a chronic care management program.
The population faces a slew of chronic conditions. Your clinic is likely familiar with many of them, but here is a list of some of the more common ones. Here are some of the conditions that qualify for chronic care management:
A CCM program helps to improve patient experiences and outcomes while boosting both your clinical value and its revenue. Whether in-house or outsourced, a CCM program should be staffed by qualified, licensed clinicians who conduct the monthly patient encounters. While the path to success varies by clinic, here are four common steps to take toward establishing a CCM program:
What do chronic care management services include?
CCM services may vary slightly by program but in general, all programs should offer licensed, clinical professionals who can coach patients with self-management for their chronic conditions such as diabetes and COPD. CCM services do so through a monthly phone call of at least 20 minutes with each patient to discuss not only overall health but also potential lifestyle changes that may benefit a patient’s longevity.
You already know that your patients will schedule an appointment with you when a health issue arises. But running your clinic this way removes your patient’s ability to take control of their own health education.
Consider a patient you have who already has asthma and obesity. He or she visits your clinic annually for a physical and wants to steer clear of additional chronic conditions like heart disease. But year after year, their health has only gotten worse. Eventually it gets to a point where you feel your patient isn’t listening to your medical advice. You wish you could check up with them on a regular basis to make sure they are following your recommendations for living a healthier lifestyle, but you simply don’t have time, and this patient gets lost in the shuffle amongst other annual patients.
A CCM program offers a “different” way to do things at your clinic. Enrolled in a CCM program, this patient would receive a monthly call to discuss their current health and the looming possibility of additional chronic conditions. They could be monitored to ensure they are taking their medications and adhering to your treatment plans, and they could be educated on the importance of nutrition as a way to improve clinical outcomes.
A CCM program offers your patients more control over their own health because they feel educated and cared for.
The following conditions must be met to qualify a patient for your CCM program:
CCM services can help change the way you interact with and care for your patients—for the better. Clinics that implement chronic care management services experience improved patient engagement which leads to better clinical results and an increased revenue stream. CCM helps healthcare teams meet the patient where they are, helping them invest in their own healthcare, and helping to knock down any barriers to their health goals.
There are various benefits—for both patients and providers— to implementing a chronic care management program into your practice.
Patients enrolled in a CCM program report stronger connections with their healthcare team. Not only will a CCM program improve patient engagement and compliance, but it also gives your team additional information behind each enrolled patient thus allowing you to see the big picture behind each patient’s current medical situation.
Additionally, CCM program patients are more likely to:
Today’s healthcare facilities already have a lot on their plate. And it’s hard to imagine giving your staff even more work to do—even if it benefits your patients. The good news is that a chronic care management service doesn’t need to be difficult or stressful to implement. And when done correctly, a good CCM program not only offers your providers valuable insights on patients, but it also creates a more streamlined approach to patient care.
We painted a rosy picture of the benefits of CCM programs for your patients. But there are challenges that can be associated with implementing one. It’s up to you to decide if the following challenges your patients may face are worthwhile to overcome.
Some CCM program patients will face the following obstacles:
As with the challenges of a CCM program that may arise for patients, physicians at your clinic may also face obstacles. The good news is that because these issues are often similar across practices, a good CCM program partner is familiar with them and may offer some reprieve.
Some CCM program physicians will face the following obstacles:
Up until recently, there was only one “type” of CCM program. However, as COVID-19 became more prevalent, concern grew for older patients with existing chronic conditions. Not only were these patients at higher risk for contracting COVID-19, making travel to their physician’s office difficult, but they also faced long stretches with little to no face-to-face interaction while in isolation from loved ones. Therefore, Remote Patient Monitoring (RPM) and Behavioral Health Integration (BHI) are now services that can be “add-ons” to an existing CCM program though they have slightly varied requirements.
Remote Patient Monitoring: Blood pressure monitors, blood glucose meters, and weight scales are all examples of common remote monitoring devices. Again, requiring consent to enroll, a patient also often pays a monthly fee for the monitoring device. A clinician must speak to patients for at least 20 minutes, up to 60. A practice can provide their own devices (self-managed) or they can contract with a company that provides devices for patients (full service).
Behavioral Health Integration: In addition to the requirements set forth by a general CCM program, a BHI adds the condition for a monthly mental health assessment.
Occasionally “CCM” is mistaken for Chronic Care Model rather than Chronic Care Management. As it happens, there is a difference. While Chronic Care Management refers to everything we’ve discussed so far, the Chronic Care Model is described as a framework which helps organizations provide care for patients that face chronic disease.
In America, chronic disease is the leading cause of death and disability among patients, and it is the leading driver of the nation’s annual healthcare costs. Chronic care management has deeply seeded roots in the chronic care model and helps providers come up with new solutions to battle through barriers, improve the outcomes of their patients, and lower the cost of healthcare, making it more accessible to Medicare patients.
Clinics may avoid a CCM program because it seems too difficult to bill. In reality, a CCM program is easy to submit for reimbursement as there are only Two main codes for primary care: 99490 or for FQHC or RHC G0511. Learn more about CPT codes and how to bill for chronic care management.
CCM services are eligible for reimbursements through Medicare when they meet conditions qualify for chronic care management, also outlined in the beginning.
The code G0511 offers a reimbursement of $76.94 per encounter (per month). Here is an example for what that may look like for your clinic:
1 patient = $76.94
250 patients x 1 call per month = $19,235
$19,235 x 12 months
$230,820 in incremental reimbursements
The code 99490 offers a reimbursement of $62.16. Here is an example for what that may look like for your clinic:
1 patient = $62.16
250 patients x 1 call per month = $15,540
$15,540 x 12 months
$186,480 in incremental reimbursements
There are three options when considering CCM software.
Your clinic already utilizes an EMR system to store patient information. Many of these offer a CCM portal within that EMR.
Purchase a CCM software that runs independently of your EMR.
Hire a trusted third-party that works within your current EMR.
Once you decide that a CCM program will benefit your patients, you face the daunting task of implementing it into your clinic. You could do it yourself in which case there are a few things you should know before you begin.
Or you have the opportunity to outsource your CCM program to a company like H3C. Because what you may already realize is that implementing a CCM program isn’t as easy as 1…2…3! Rather it’s a Herculean effort that presents looming challenges which could take weeks, months, or even years to accommodate.
The idea of handing over your patients to an outsourced company can be daunting. Will they have the same level of respect and care for your patients? Will your patients realize someone outside your clinic is contacting them? Will an outside company try to steal patient information?
And if all those concerns are satisfied, there are so many CCM program partners to choose from. How will you decide? As it turns out there are a few things that a reputable CCM program provider will have:
Outsourcing doesn’t need to equal complexity. An outsourced CCM program partner has similar goals as you do to better serve your patients. And there are a multitude of benefits to finding the right CCM partner, including no:
Outsourcing isn’t always the right fit. If you choose to implement a CCM program yourself, there are benefits to doing so, including limited risk of:
You may decide to go the route of an internal CCM program. As with outsourcing you will discover that there are numerous benefits and challenges associated with your decision. Once you’ve given each their due, you can decide what route is better for your clinic—in-house or outsourcing?
Keeping your CCM program in-house comes with numerous pluses such as:
Naturally, keeping your CCM program in-house also comes equipped with challenges. Some of the more common ones include:
When you choose H3C as your chronic care management partner, we make it easy to implement a CCM program into your existing practice. Here’s how it will work.
From there, we do everything in our power to make your life (and the lives of your patients) better.
At H3C we offer a variety of services designed to make outsourcing your CCM program the easiest decision you will ever make. Our team of experts covers:
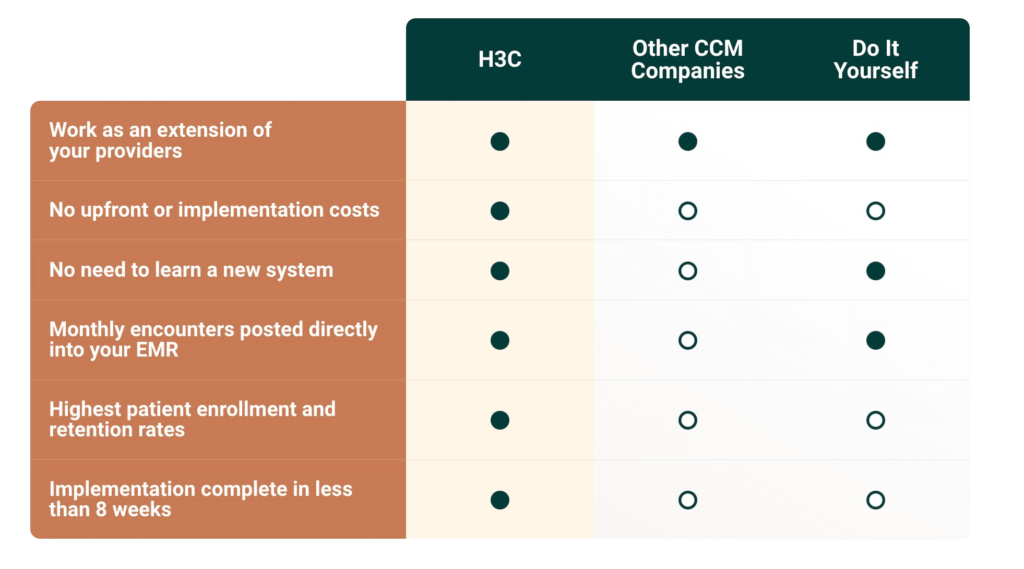
It’s true, H3C isn’t the only company that can help you with your CCM program. But when we choose to work together, know that H3C has a long history of working with top-notch organizations like yours and we have a reputation for delivering consistent, high-quality results for each and every one of them.
At H3C, not only do we provide our CCM program and technology at no cost to clinics, but we also help generate additional revenue to improve clinics and the care they provide. Come learn why clinics like yours trust us to provide top-level care for their patients. Connect with H3C today.
Chronic care management focuses on serving individuals on Medicare with two or more chronic conditions. CCM is a preventative service, helping your Medicare patients take a proactive approach to their health and wellness, while keeping them connected to their provider.
Here are some of the conditions that qualify for chronic care management:
In 2022, G0511, the CPT code used by FQHCs and RHCs, will carry a reimbursement of $76.94 per encounter (per month), an increase of $11.70 or 18% over 2021 reimbursement levels.
The reimbursement rate for CPT code 99490 (the CCM look-alike code for non FQHCs/RHCs) will also be increased in 2022 from $41.17 to $62.16, a year-over-year increase of 50%.
Medical offices that meet the following conditions can bill for a CCM program:
This is CCM performed via phone call
Any federally qualified health center, rural health clinic, or critical access hospital can bill for CCM services.
CCM bills must be submitted at 30-day intervals. If a bill falls outside this timeline, it may not be accepted for reimbursement.
No. At this time, CCM programs only require consent to be given prior to enrollment.
A CCM nurse may handle a variety of tasks including performing CCM calls and handling all corresponding communication aspects, virtual assistance in helping patients manage their chronic conditions, responding to incoming calls from CCM patients and offering medication or treatment instructions to patients and their families.
What’s right for you?Outsourcing your Chronic Care Management program to H3C turns an ongoing expense into a revenue generator. Plus, you’ll make your patients’ lives better with more regular communication between visits.